Oncology induction booklet was contributed by the following;
written by Dr Pearce and Dr Kaur
Reviewed by Dr Fernandes
Updated by Dr Amir Shenouda
Select the booklet titles below to expand the table to view more information.
Oncology Commitments
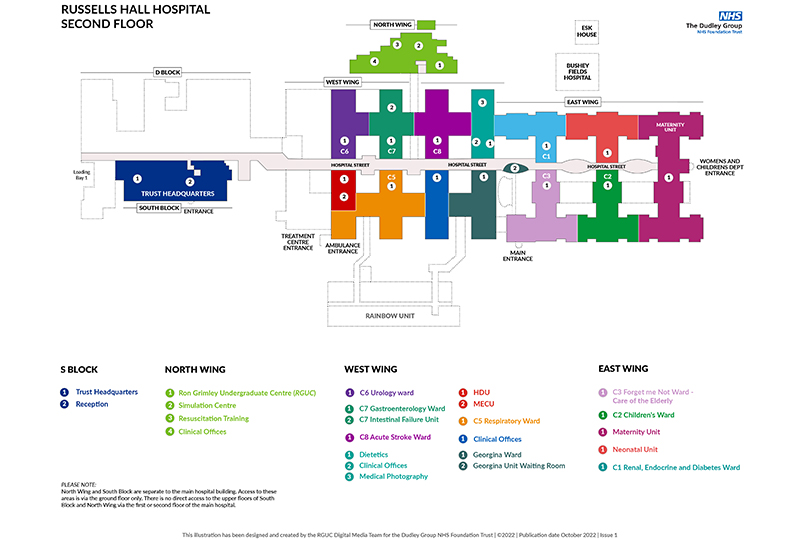
C4 Georgina Ward
Each day will involve conducting a ward round of any patient admitted under oncology on C4 Georgina ward. Patients will only be admitted under oncology if they are known to a “visiting” DGH Trust oncology consultant. The consultants are not based at Russell’s Hall Hospital (most are based at New Cross Hospital), but instead will have one or two oncology clinics on C4 each week. They will not automatically review their patients if they are admitted onto the ward so you will perform your ward round with an oncology registrar, Dr. Pamma.
Acute Oncology Service (AOS)
After reviewing the patients, you will then be responsible for ensuring that any jobs created are completed. If a patient has not been seen by an oncology consultant during their admission, you will need to liaise with the ‘Acute Oncology Service’ (AOS) for senior input. AOS generally consist of clinical nurse specialists and an oncology consultant.
AOS perform a ward round of patients referred with acute oncological problems from anywhere in the hospital. For example, oncology patients who are not known to a DGH Trust Oncology consultant (e.g., their consultant is based at the QE), will be admitted under General Medicine, and will need the AOS team to review.

Oncology - Triage
Triage Services

Both haematology and oncology patients have access to the triage service which runs from C4 09:00-17:00 Monday to Friday, and also on the weekend – however you only cover the week day service. Furthermore, at 16:00 the triage service will refer any patients requiring in-patient assessment to the acute medical unit downstairs as this allows you to finish with the remaining patients till 17:00.
The triage service runs from a desk on C4 in between day case and the isolation unit. Patients will phone through to the nurse sat beside you and run through a standard set of questions on their proforma, and make a decision where to go from there. Occasionally they can give advice without needing to consult with you, or they will advise they need to consult with a doctor and will discuss with you on how to proceed. If this is the case it can include simply writing a prescription (e.g. laxatives), or a more in-depth review requiring a full history and examination in which you would call the patient in to attend the ward.
Triage is allocated two corner spaces in the day case unit that have stretchers to assess patients on – as the rest of day case has chairs.
Common queries include side effects from chemotherapy such as nausea, vomiting, constipation, diarrhoea, a sore mouth or chemotherapy specific side effects. When assessing these presentations, it is about determining the severity.
Select the titles below to find out further information.
For example, with nausea they may have just finished their course of post-chemotherapy anti-emetics (usually dexamethasone + ondansetron) and require more as still feeling the side effects in which a prescription may suffice. However, if they are vomiting and not tolerating any food or fluids they will need to be admitted for intravenous fluids and anti- emetics.
With regards to mouth care, all patients should be on chlorhexidine QDS already. Other treatments that can be given include Difflam mouth wash (more analgesic), and Gelclair. Gelclair is 1 application TDS – not easily found in the BNF. When assessing patients post- chemotherapy, it is important to check for thrush as this is very common and will require treatment.
If patients are suffering from constipation – start by assessing how much of any laxatives prescribed they’ve had including those over-the-counter. Occasionally they may have 4 sachets of Movicol in a day – as the normal prescription is 2 sachets a day. Conversely, if a patient is suffering from diarrhoea it will be determining the severity such as the need for resuscitation with fluids and ruling out an infective cause with cultures given their immunocompromised state.
Any patient that has a temperature spike at home will automatically be asked to come in to check their blood counts as there is a risk of febrile neutropenia and neutropenic sepsis. The Georgina Unit handbook (on the Hub – type in ‘Georgina Unit Haematology Handbook) includes the protocol for neutropenic sepsis whereby it is the same as sepsis 6 – however cultures may also need to be taken from any lines in-situ and the antibiotic of choice may be different. Refer to the Georgina Unit Handbook for current antibiotic choice.
Rashes can be quite specific to certain chemotherapy agents – if you are unsure it is always best to run through with a senior. Knowledge will build up with time and you are not expected to know lots of detail about each chemotherapy agent.
Bisphosphonates are commonly given to patients with myeloma and it is important to rule out osteonecrosis of the jaw should any patients present with jaw pain. Therefore, requesting an OPG and maxillofacial review should cover this as any dental work required is usually done under their team due to immunocompromised status.
Oncology Day Case
Triage

Part of triage is also covering the day-case unit where patients attend to have their chemotherapy. This is nurse-led with appointments pre-booked. Occasionally nurses will present with queries about whether to proceed with a patient’s treatment today.
Getting a good background of the patient helps deal with these queries. For example, try to ascertain the following details:
- Diagnosis
- Any metastases
- What the chemotherapy is for (E.g. palliative)
- Baseline health usually
- Baseline health post chemo
- Latest development in management – g. Scans
Assessing the patient
After acquiring the above details, you can go and assess the patient to see where their health is currently sitting at. For example, if the nurse reports the patient has a cough – it might be a simple lower respiratory tract infection, or the patient’s primary is lung cancer and they usually have a cough but it is more troublesome than usual.
If patients have an infection usually chemotherapy is deferred by 7 days and treated in the meantime. FY1s cannot make decisions regarding chemotherapy. Once you have assessed the patient, you must discuss it with a senior who will advise you whether the patient needs their chemotherapy deferring or not. Speak to Dr Pamma for Oncology patients and Dr Aurangzeb for Haematology patients. The haematology consultants are also happy to advise.
Bloods
Other queries can include deranged blood results as all patients have pre-chemotherapy bloods the day before. It helps to assess the trend of the patient’s bloods with their latest investigations/letters rather than look at the last results. For example, between their last cycle and second cycle their ALP may have risen – however if you search for their latest CT staging scan it may have revealed new liver metastases. Deranged electrolytes are also very common and the aim here is to assess if patients are symptomatic and no ECG changes for those that are relevant – E.g. Hyper/hypokalaemia.

ECHO
Another common request from day case staff is signing for ECHO requests. Female patients with breast cancer treated with Herceptin need regular ECHOs to ensure their ejection fraction is preserved. Nurses will usually have filled out all the required details and need your signature to request the ECHO.
Oncology Commitments
C4 Georgina Ward
You will be expected to complete jobs, discharge summaries and referrals for any of the general medical outlier patients situated on C4. A medical consultant, Dr. Bilal, or a member of his team (e.g. registrar Redstone), will attend the ward and review patients admitted under General Medicine. As these are outlier patients, the medical team are not based on the ward all of the time, but you can contact them via switchboard. You may be too busy with your oncology commitments to attend his ward round, but you will be expected to complete the jobs for medical patients.

Health and Wellbeing
Staff that are happy and thriving in their working environment will inevitably have a more enjoyable experience in the workplace, contributing to the provision of excellent health care for all of our patients. The Dudley Group recognises our commitment to staff wellbeing in a variety of ways.
Select the link below to find out more how the Trust can support you.